Ronaldo Araújo Souza, João da Costa Pinto Dantas, Suely Colombo, Maurício Lago, José Antônio Poli de Figueiredo and Jesus Djalma Pécora analyse the relationship between the apical limit of root canal filling and the repair of periapical lesions.
Introduction
Inadequate apical limit of root canal filling has been pointed out as one of the most important prognostic factors related to apical periodontitis and its acute symptoms among root canal-treated teeth (Kim, 2010; Guinesi et al, 2014; Holland et al, 2017).
The persistence of peri-radicular inflammation might be attributed to continuing apical percolation of serum, bacteria and its breakdown products (Ingle, 1956; Sjögren et al, 1990; Nguyen, 1994). Stagnancy and release of toxic substances by tissue fluid seeped into the empty space in the apical third of the canal would be the main cause of periapical lesion (Ingle, 1956; Sjögren et al, 1990; Nguyen, 1994).
Owing to the presence of microorganisms in the root canal system and to the lower probability of success, still greater importance has been attributed to root canal filling when treating teeth with periapical lesions (Wu, Wesselink and Walton, 2000). According to Nguyen (1994), unless a dense, well-adapted root canal filling is achieved, the prognosis may be jeopardised, regardless of how well other phases of the treatment are carried out. Hermetic seal has long been considered the most important goal for success in endodontics (Sjögren et al, 1990). In order to achieve a hermetic seal, the root canal should be filled up totally to the radiographic apex or as close to it as possible. Despite the lack of consensus on these limits, the majority of authors suggest filling the root canal 1 mm short of the apex. More recently, coronal leakage, rather than a lack of apical seal, has been pointed out as the main cause of endodontic treatment failure (Ray and Trope, 1995), but this is still a point of controversy (Kim, 2010).
Considering these still undefined parameters, the aim of this work was to analyse the relationship between the apical limit of root canal filling and the repair of periapical lesions.

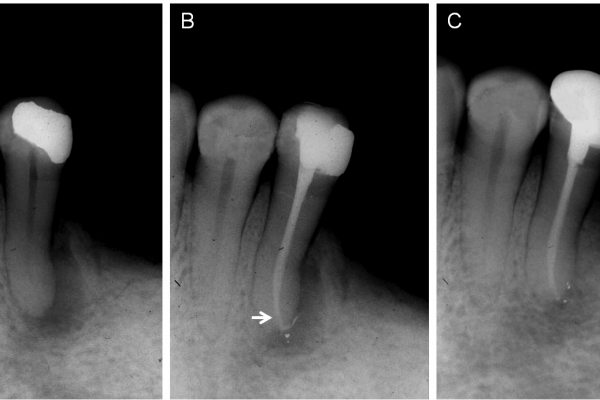
Figure 1: Control group
Figure 1a: Initial radiograph of the maxillary right lateral incisor showing a large periapical lesion
Figure 1b: Root canal filling 1 mm short of the apex
Figure 1c: A two-year radiographic follow-up showing repair of the periapical lesion
Material and methods
Eighteen male and female patients (20 teeth) participated in this study. Aged 25-45 years, the patients were not being treated with antibiotics and had no systemic diseases, such as uncontrolled hypertension and uncontrolled diabetes mellitus. Informed consent was obtained from each of them after the clinical procedures were thoroughly explained.
A complete clinical record was maintained for each patient, containing the chief complaint, clinical and radiographic aspects of the teeth, results of pulp sensitivity and percussion tests, as well as the endodontic procedures performed. All clinical procedures were carried out by one experienced endodontist in a private practice from 1987 to 1996.
Teeth excluded from the study had incomplete formed apices, confirmed by radiographic evaluation, or the presence of accidents or complications during treatment (calcified canals, impossibility of achieving foraminal patency).
There was no specific criteria for inclusion, except for the fact that all of them had periapical lesions measuring no more than 8 mm in diameter. After local anaesthesia, carious dentine was excavated and the teeth were isolated with a rubber dam. Thorough disinfection of the teeth and the rubber dam was done by using 2.5% NaOCl, and the endodontic access cavities were prepared with sterile high-speed carbide burs.
The working length (WL) was radiographically established at 1 mm short of the apex for all the teeth. Canals were initially instrumented by using manual watch-winding motion with #10 and #15 K-file (Dentsply Sirona Maillefer) and then were coronally flared by using Gates Glidden burs sizes 1, 2 and 3. Hand instrumentation was continued with an adjusted K-file at working length and four additional K-files of progressively increasing diameters.
Throughout the preparation the root canals were irrigated with 2 ml of 2.5% sodium hypochlorite at each file change, by inserting the irrigation needle 6 mm short of the apex, and foraminal patency was performed with a #10 K-file placed 1 mm beyond the WL (Souza, 2006) (Figures 4a, 5b, 5d and 6b). After preparation of root canal, instrumentation of the cemented canal was performed in all of the teeth by using manual watch-winding motion with a file that was bound to the walls of the foramens (Souza, 2006). Root canals were then irrigated with 3 ml sterile saline, with the irrigation needle positioned at 3 mm short of the apex, and dried with sterile paper points (Tanari, Manaus, Brazil).
Control group
Figure 2a: Initial radiograph of the maxillary right lateral and central incisors with periapical lesions
Figure 2b: Root canal fillings were performed 1 mm short of the apex in both canals. Observe that despite the overflow of sealer in the central incisor, the master Gutta Percha cone was positioned 1 mm short of the apex (arrow)
Figure 2c: Five-year follow-up radiograph shows complete repair on the lateral, but incomplete repair on the central incisor
Control group
Figure 3a: Initial radiograph of the mandibular left second bicuspid with periapical lesion extending laterally
Figure 3b: Despite the sealer overflow, the Gutta Percha cone remained 1 mm short of the apex (arrow)
Figure 3c: Two-year follow-up shows incomplete repair
For smear layer removal, canals were flooded with 1 ml of 17% EDTA (Inodon, Porto Alegre, Brazil), which was stirred with a Lentulo spiral (Dentsply Sirona Maillefer) and then allowed to remain in the canals for three minutes. After that, canals were irrigated with 3 ml of 2.5% sodium hypochlorite, which was also stirred with a Lentulo spiral and left in the canals for five minutes. Finally, the root canals were rinsed with 4 ml of sterile saline solution, dried with sterile paper points, and dressed with a freshly prepared paste of calcium hydroxide in sterile saline carried by a Lentulo spiral. The paste was condensed at the canal orifice level with the aid of sterile cotton pellets and pluggers. A sterile cotton pellet moistened in saline solution was used to clean the pulp chamber walls from calcium hydroxide residues and access cavities were closed with intermediate restorative material (IRM). The intracanal dressing was initially left in the canal for 21 days and then renewed twice, at 30 and 60 days after the first dressing. After these periods, the patients were anaesthetised, rubber dam was applied, the operative field was disinfected as described, and the root canals were reinstrumented with the last instrument used at the WL, with an irrigant of 5 ml of 2.5% NaOCl. A final rinse was carried out with 4 ml of sterile saline solution and the canals were dried with sterile paper points. Root canals were divided in two groups. In the control group (n=10), they were filled 1 mm short of the apex and in the experimental group (n=10), to limits ranging from 2 mm to 7 mm short of the apex. Root canal filling of both groups was carried out by lateral condensation of Gutta Percha (Tanari, Manaus, Brazil) and Fill Canal (DG Ligas Odontológicas Ltda, Rio de Janeiro, Brazil), a zinc oxide-eugenol sealer. After obturation, excess material was removed from the pulp chamber and the access cavities were sealed with IRM.
Patients were followed up from one to 21 years after treatment was completed. Three radiographic aspects were considered to assess treatment outcome:
1. Complete healing (new bone formation and reestablishment of anatomic reference points – lamina dura and periodontal ligament width)
2. Incomplete healing (decrease in lesion size)
3. Failure (persistence or enlargement of the lesion). Data was statistically analysed by Fisher’s exact test.
Results
• There was no statistical difference between the groups (Table 1).
• Control group: root canals filled 1 mm short of the apex (n=10).
• All 10 cases showed some degree of repair: complete healing was observed in eight teeth (Figure 1), and incomplete healing in two cases (Figures 2 and 3).
• Experimental group: root canals filled from 2 mm to 7 mm short of the apex (n=10).
• All 10 teeth presented complete healing (Figures 4-8).
Discussion
It was once believed that empty spaces created by incomplete root canal fillings were the predominant cause of endodontic treatment failures (Holland et al, 2017). More recently, the prevalence of periapical lesions was found to be significantly higher among underfilled root canals, and the authors concluded that considerable effort should be made by dental practitioners to improve the technical quality of root canal fillings (Özbaş H, Aşcı S and Aydın Y, 2011).
This theory, however, was not corroborated by this current study, given that the empty spaces left after obturation in the experimental group did not interfere with the healing process. No significant difference was observed between the teeth in the control group, where root canals were obturated 1 mm short of the apex, and those in the experimental group, where fillings were made very short of the apex. In addition to periapical healing, we observed repair by deposition of mineralised tissue, as depicted in Figures 4c, 4d, 5f-5g, 6g, 6h and 7e.
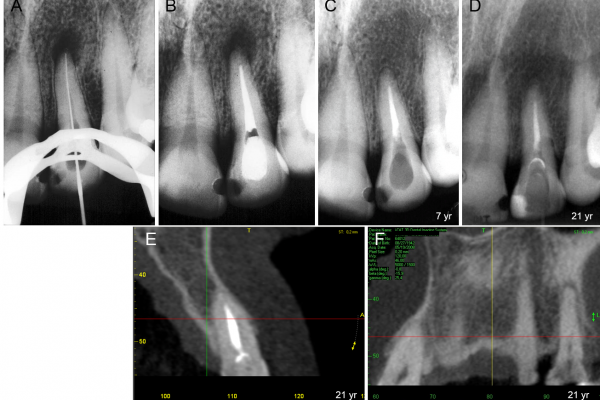
Experimental group
Figure 4a: Radiograph showing that the entire extension of the canal of the maxillary left lateral incisor was instrumented, including the apical foramen
Figure 4b: Root canal filling performed in 1987 up to 4 mm short of the apex
Figure 4c: Seven-year follow-up shows resolution of the periapical lesion
Figure 4d: 21-year follow-up confirms repair of periapical lesion observed in Figure 4c
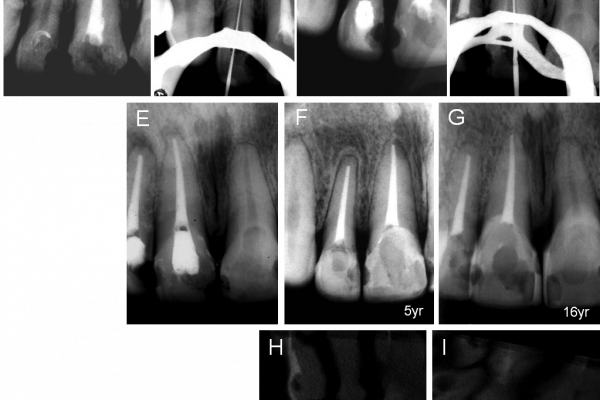
Figure 5: Initial radiograph of the maxillary right central and lateral incisors, both with periapical lesions and root resorption on the apex of the lateral incisor
Figure 5b: The entire extension of the canal in the lateral incisor was instrumented, including the area of resorption in the cemented canal
Figure 5c: Root canal filling of the lateral incisor was done 2 mm short of the apex (experimental group). Observe the apical resorption
Figure 5d: Retreatment of the central incisor, showing the file at the apical foramen
Figure 5e: Obturation of the central incisor 1 mm short of the apex (control group)
Figure 5f: Regardless of the different apical filling limits and of the pathology detected (apical resorption on the lateral incisor), both teeth showed repair five years after endodontic treatment. This patient had previously undergone orthodontic treatment
Figure 5g: A 16-year follow-up radiograph confirms repair
Figures 5h and 5i: CBCT confirms repair of the periapical lesions observed in Figure 5g

Experimental group
Figure 6a: Initial radiograph of the mandibular right central incisor showing large periapical lesion and apical foramen resorption
Figure 6b: The area of resorption in the cemented canal was instrumented by Hedstrom file
Figure 6c: Root canal dressed with calcium hydroxide. Note the similar radiopacity of calcium hydroxide and dentine
Figure 6d: Fitting the master Gutta Percha cone at the ‘ideal’ length
Figure 6e: Fitting the master Gutta Percha cone very short of the apex
Figure 6f: Root canal filling 6 mm short of the apex. Note the slight sealer overflow beyond the master Gutta Percha cone (white arrow), the width of the apical portion of the canal after preparation (black arrow), and the resorbed foramen (arrowhead)
Figure 6g: A five-year follow-up image shows the ongoing repair of the periapical lesion, disappearance of the sealer that had leaked beyond the master Gutta Percha cone (white arrow), and apical remodeling. Note the deposition of mineralised tissue (black arrow) with mineralisation of the apical portion of the canal seen in
Figure 6f: (black arrow)
Figure 6h: An 11-year follow-up shows periapical lesion repair, apical remodeling, and increased deposition of mineralised tissue (arrow)
Figures 6i and 6j: CBCT confirms repair of the periapical lesion
Our observations are in agreement with the findings of Torneck (1966), that empty spaces in incomplete root canal fillings do not induce treatment failure. They also corroborate the results from Sabeti et al (2006), who compared dogs’ teeth with periapical lesions subjected to endodontic therapy and did not find significant difference between teeth with filled canals and those left empty.
There are important factors that should be analysed. Figure 6f shows the radiograph of the mandibular right central incisor with slight overflow of sealer cement beyond the master Gutta Percha cone. After five years, this material was no longer visible (Figure 6g). According to the literature, disappearance of the sealer that had leaked beyond the master Gutta Percha cone would support the idea of leakage of tissue fluids through empty spaces, which would prevent the periapical lesion repair. However, repair was observed five and 11 years later (Figures 6g and 6h).
In another case, the root canal filling in a mandibular left first molar presented empty space close to the fractured file (Figure 8a) and two years and eight months later there was considerable loss of filling homogeneity and increase on the size of the periapical lesion (Figure 8b). Due to the lack of hermetic apical seal, tissue fluids probably seeped into the canal, dissolving the sealer (visualised as loss of filling homogeneity), and as a result of stagnation and decomposition, toxic substances would have been released into the periapical tissues, leading to the increase in lesion size. These observations corroborate previous studies that attribute endodontic therapy failure to empty spaces left in the canal after incomplete obturation (Holland et al, 2017; Ingle, 1956; Sjögren et al, 1990; Nguyen, 1994; Özbaş et al, 2011).
According to those studies, it would be expected that the presence of a fractured instrument combined with the intentional 5 mm space left between the obturation and the apex (Figure 8f) would promote conditions leading to fluid leakage and consequent stagnation, decomposition and generation of toxins. However, repair was observed after two years (Figure 8g), the same amount of time as the maxillary right lateral incisor shown in Figure 1, where the canal was filled 1 mm short of the apex (control group). There are no clinical studies in the endodontic literature that consistently show the relationship between apical limit of root canal filling and repair of periapical lesion. Maybe a limitation is the difficulty to conduct this type of study. In this work, two major difficulties were observed:
1. To obtain the consent from the patients, which explains why it took so long (10 years) to get a minimum of cases
2. To keep them for a long term follow-up. One of the consequences is that clinical studies usually present small sample sizes. This was also a problem for the present study and as a consequence statistical analysis was not really useful.
Anyway, despite the lack of statistical significance between the groups, complete healing was less frequent in the control group, where the root canals were filled 1 mm short of the apex. In this group, sealer overflow occurred in two canals (Figures 2b and 3b).
Previous studies have demonstrated the interference of obturating material extrusion in the repair of periapical lesions (Ricucci et al, 2011), which probably explains the absence of complete repair in the teeth shown in Figures 2c and 3c. It is also possible that the greater proximity of the filling limit with the apex may have favoured the extrusion of sealer. Radiographs in Figures 2c and 5f were taken with a five-year interval, and the difference in quality of repair is evident when the images are compared.
Therefore, it appears to be a misconception to recommend that fillings should be flush to the apex or, even worse, with periapical extrusion, as a proof of obturation quality and necessary procedure to obtain repair. Besides not ensuring therapeutic success, these procedures may delay or even prevent healing of periapical lesions.
Once it apparently seems that the apical limit of the obturation is not the determinant factor for periapical repair, it does not appear to be an adequate premise to attribute endodontic success to either filling technique or obturating material (Ricucci and Siqueira, 2010). Filling techniques and materials present certain characteristics that make them more appropriate for use in specific situations, but cannot be held responsible for the presence or absence of repair.
Comparison of Figures 2, 5, and 6 further demonstrates this fact. In the five-year period between Figures 2b and 2c, repair was incomplete, probably due to the presence of extruded sealer. The same period of time had elapsed between the images shown in Figures 5c and 5f, 6f and 6g, all of which show complete healing of the periapical tissues.
The participation of microorganisms in the development of pulpal and periapical tissue diseases is established (Kakehashi et al, 1965; Fabricius et al, 2006; Chávez de Paz, 2007; Vera et al, 2012), and the main biological factor influencing the outcome of endodontic treatment appears to be the extent of microbiological insult to these tissues (Chugal et al, 2003). Eradication of microorganisms from an infected root canal system has been demonstrated as the key to successful endodontic treatment (Chugal et al, 2007).
It should be understood that healing occurs when the causal factor of the disease is removed. In endodontics, this is accomplished by elimination of bacteria (infection control) from the root canal system, which is the role of root canal preparation, not of endodontic filling. Root canal filling is certainly an important step to achieve a seal and maintain the infection control accomplished by root canal preparation, but the results of this study do not show that it can be considered as the determinant factor for success (Sabeti et al, 2006; Souza et al, 2011; Figdor, 2002).
While recent technological developments have been valuable and most welcome, the strong emphasis on techniques in modern endodontics has no doubt detracted attention from the primary aim of endodontic therapy, which is to prevent or treat endodontic infections. As a result, less weight appears to have been placed on the means by which root canal infections can be controlled (Bergenholtz and Spangberg, 2004).
Some important final considerations should be made. Firstly, it should be highlighted that in the present work, regardless of the apical obturation limit, each canal was instrumented in its entire extension, including its cemented portion (Souza, 2006; Souza et al, 2011; Souza et al, 2012) (Figures 4a, 5b and 5d, 6b and 8c).

Experimental group
Figure 7a: Initial radiograph of the mandibular left second molar, with large apical resorption of the distal root
Figure 7b: Establishment of the working length (WL) in the mesial and distal canals during retreatment. In the distal canals, files are at the working length where shaping, cleaning, and root filling were performed, but they were debrided beyond those measurements, up to the ‘old’ apex for cleaning the entire extension of the canal, including the resorbed portion (arrow)
Figure 7c: Master Gutta Percha cones at the working length in the distal and mesial canals
Figure 7d: Root canal filling. Note that Gutta Percha cones (arrow) are very short of the ‘old’ apex. Beyond this point sealer overflow was detected
Figure 7e: A five-year follow-up shows remodeling of the distal root, with a new outline (white arrow). Note that the master Gutta Percha cones are 7 mm short of the apex (black arrow)
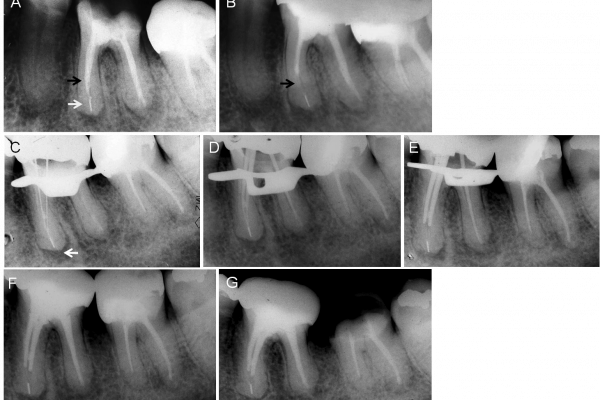
Experimental group
Figure 8a: Initial radiograph of the mandibular left first molar, showing a fractured instrument at the apex (white arrow) and periapical lesion. Note the density of the root canal filling (black arrow)
Figure 8b: Radiograph taken 2.8 years later shows increase in the size of the periapical lesion and lack of homogeneity of the root canal filling (arrow), compared with Figure 8a
Figure 8c: Image of mesial and distal canals during retreatment, showing a 15-flexofile instrumenting the apical foramen in the mesial canal (arrow)
Figure 8d: Fitting of the master Gutta Percha cones. Note that in the mesial canals, the Gutta Percha cones reach the fractured file
Figure 8e: Fitting of the master Gutta Percha cones was done at 5 mm short of the apex in the mesial canals
Figure 8f: Root canal filling completed and intentionally filled 5 mm short of the apex in mesial canals
Figure 8g: A two-year follow-up radiograph shows repair of the periapical lesions
The second consideration that should be made clear is that we do not aim to imply that root canal obturation is an unimportant step or that it can be carried out carelessly. Apical limit of root canal fillings should be what is established by endodontic literature, about 1 mm short of the apex according to majority of the authors. Our real goal is to highlight the importance of infection control for endodontic success (Ricucci and Siqueira, 2010; Vera et al, 2012; Bergenholtz and Spangberg, 2004).
Conclusion
Despite the relatively small sample size, results suggest that the apical limit of obturation seems to have no influence in the repair of periapical lesions. Our results point towards the notion that root canal preparation appears to be the determinant factor for periapical lesion repair. Further clinical studies on this subject are needed.



