Sensodyne explores the best ways to maintain compliance amongst patients.
Sensodyne explores the best ways to maintain compliance amongst patients.
There are a number of oral care conditions where resolution may rely on patients’ actions between dental appointments, as opposed to treatment in the dental chair. Dentine hypersensitivity is one such condition. Although there are potential in-surgery management options, the first line of non-invasive treatment tends to be the recommended use of a desensitising toothpaste twice daily (Canadian Advisory Board on Dentin Hypersensitivity, 2003).
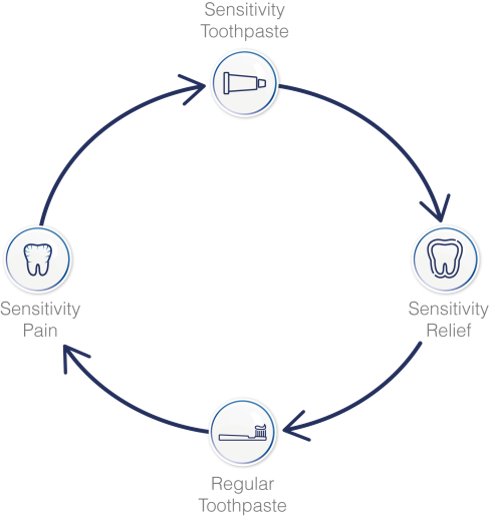
The dentine hypersensitivity pain cycle
The use of a desensitising toothpaste has been a recognised treatment option for the condition of dentine hypersensitivity since the launch of brands, such as Sensodyne, in the 1960s. The recommendation is for twice daily use to stop the pain of the condition, either through an occlusive mode of action or by nerve depolarisation. However, over the years patients are often observed stopping treatment when the pain subsides, only for it to return some time later.
So how can we engage patients to comply with the recommendations for the management of dentine hypersensitivity with a daily desensitising toothpaste?
A review from the patient’s perspective
A review paper undertaken by Jing Jin et al (2008) at the University of Newcastle in New South Wales, Australia, sought to explore and evaluate the most common factors causing therapeutic non-compliance from studies across a number of countries, including different diseases and different patient populations. Some of these learnings can provide useful insights to consider for recommendations in practice.
Factors that influence levels of compliance were found to include:
- Patient demographics including age – a low compliance rate was identified for middle-aged patients and those under 40, due to other life commitments including work, which can take priority
- Educational level – it is often assumed that patients with a higher education are more capable of understanding conditions and treatments and are therefore more likely to comply. However, the review highlighted that education level was not a good predictor of the therapeutic compliance
- Marital status – the review found that, in some cases, married patients were more compliant, which may reflect the importance of a second person’s support in maintaining a treatment regime, although this was not universal
- Patient beliefs and motivations about the therapy were shown to have a part to play. The review highlights that better compliance is achieved when patients:
- Believe they are susceptible to the condition or the complications
- Are aware of the potential consequences of non-treatment
- Believe the therapy will be effective or can see the benefits.
Misconceptions about the disease or treatment have been shown to have a negative effect on compliance. One example is where patients feel that continued use of a treatment will diminish the effectiveness of that therapy.
- Patient education was found to be crucial for compliance, and the content of the education, crucial – a lack of understanding of the condition or treatment and the need to continue treatment may mean patients stop using it to see if it is still needed
- Duration of treatment period has been shown to affect compliance – in some cases people are more compliant for acute conditions and compliance can be adversely affected by longer duration of illness and treatment
- Patients with an absence or fluctuation of symptoms may have poor compliance – for example for patients with hypertension the advice to reduce levels of sodium was undertaken by 71% of patients who suffered symptoms and just 7% of those who didn’t.
So, what does this mean for patients with dentine hypersensitivity?
The review was based on 102 articles and although they were often amongst patients with more significant health concerns, there are insights that could be applied when recommending the use of a daily specialist toothpaste for DH sufferers:
- Where possible, provide information to inform patients about the causes of dentine hypersensitivity, the reasons for daily management and the potential impacts of non-treatment, ie discomfort which can impact on lifestyle and oral care. This can be verbal information, supported with leaflets. Information for professionals can be found at gskhealthpartner.com
- Explain to patients that during treatment, symptoms will subside but it is important to continue use because otherwise symptoms will return – reassure them that continued use will not make treatments less effective
- Consider the patient’s lifestyle – are they likely to have social and work demands which may reduce compliance? How could you help reinforce the importance of daily management?
- Support patients to commence treatment as soon as possible by providing a sample as part of the visit.
Whilst not life threatening, there is evidence that dentine hypersensitivity can significantly impact a patient’s quality of life (Baker et al, 2013; GSK data on file RH01897, August 2014). A daily recommendation of a specialist toothpaste can make a genuine difference and, when used correctly, reduce the impact of triggers such as cold food and drinks. There is an opportunity to consider the factors that influence compliance to help improve outcomes for patients with dentine hypersensitivity. It is therefore important to stress the need to continue treatment at each visit.
References
Baker S, Gibson B, Sufi F, Barlow A and Robinson P (2013) Longitudinal validation of the DHEQ. Poster presented at IADR/AADR/CADR General Session & Exhibition March20-23, Seattle, Washington
Canadian Advisory Board on Dentin Hypersensitivity (2003) Consensus – Based Recommendations for the Diagnosis and Management of Dentin Hypersensitivity. J Can Dent Assoc 69(4): 221-6
Jing J, Sklar GE, Oh V and Li S (2008) Factors affecting therapeutic compliance: A review from the patient’s perspective. Therapeutics & Clinical Risk Management 4(1): 269-86