 Kreena Patel kicks off her endo expert column with tips for locating and treating the MB2.
Kreena Patel kicks off her endo expert column with tips for locating and treating the MB2.
I am excited to have been invited to write a column for Dentistry Online. Each month, I will discuss different endodontic topics, present clinical cases and review some of the latest endodontic gadgets.
The MB2
The mesial-buccal 2 (MB2) or ‘fourth’ canal has quite the reputation for being challenging to locate and negotiate. This month I would like to focus on discussing facts about the MB2 and clinical tips for successfully managing it.
Importance
Just how important is this little canal? Clinicians often debate this question. Some feel they can carry out root canal treatment without treating MB2.
Successful endodontic treatment relies on locating, disinfecting and obturating all the canals. Studies have shown the incidence of MB2 canals is roughly 90% in maxillary first molars and 60% in maxillary second molars. Therefore, the majority of maxillary molars contain four canals. So we should start root canal treatment of these teeth with this in mind.
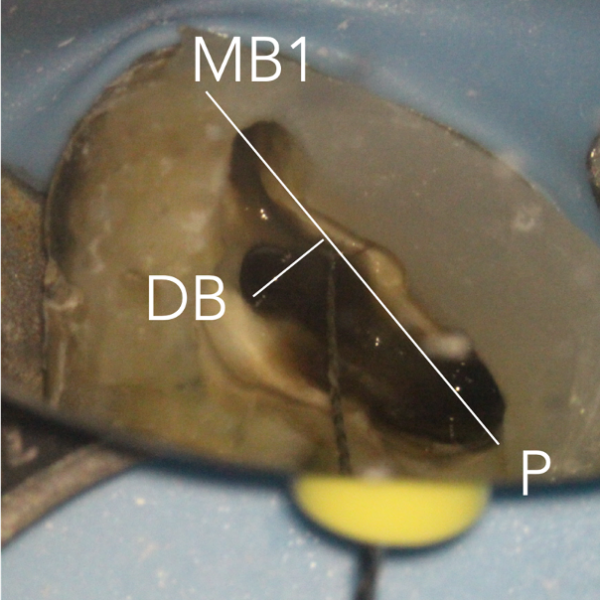
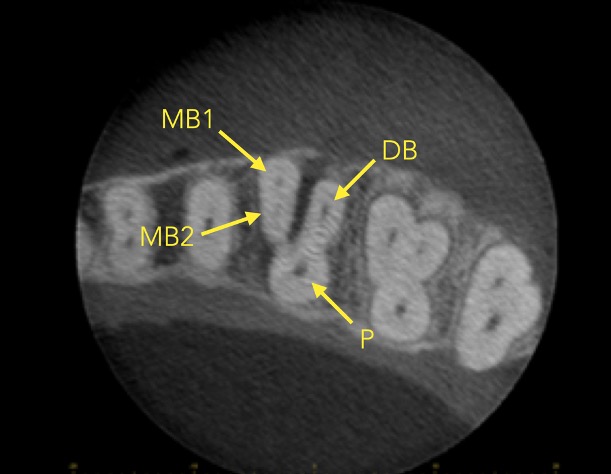
There are often multiple ports of communication between MB1 and MB2. The MB2 can join MB1 along its path or terminate via a separate apical foramen (Figures 1 and 2). Rarely, there can be an MB3 canal present (Figure 3).
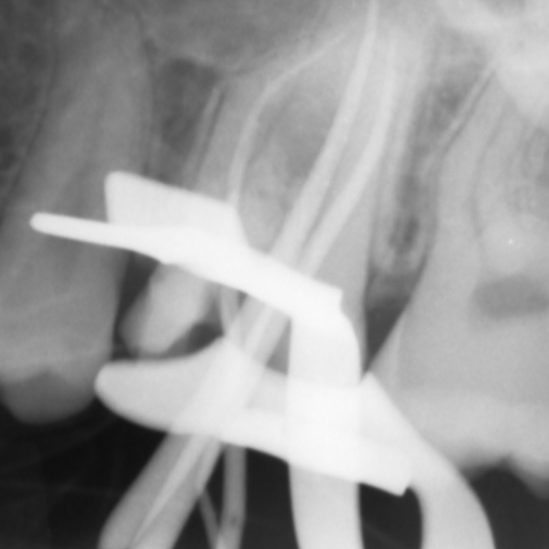
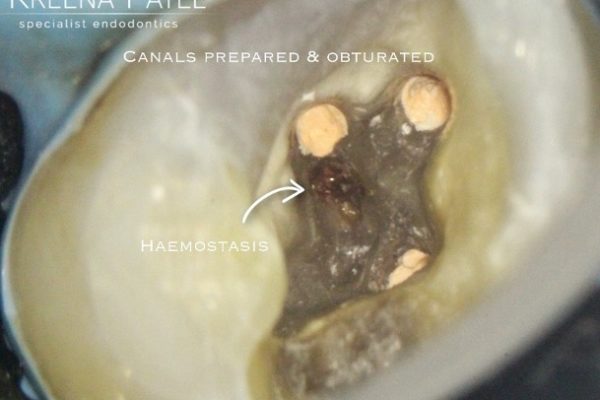
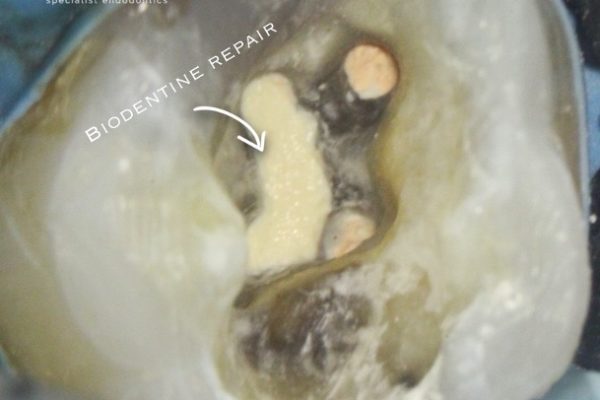
A missed MB2 canal is one of the main causes of endodontic failure in maxillary molars. In cases of irreversible pulpitis, it is responsible for ongoing temperature sensitivity. In necrotic cases, residual bacteria will increase the risk of infection (Figure 4).
Figure 1: MB1 and MB2 are two separate canals.
-
-
-
- Preoperative radiograph
- Mid-fill radiograph showing MB1 and MB2 are completely separate canals with individual apical foramen; both canals have acute apical curvatures
- Postoperative radiograph; a lateral canal was noted in the palatal canal.
-
-
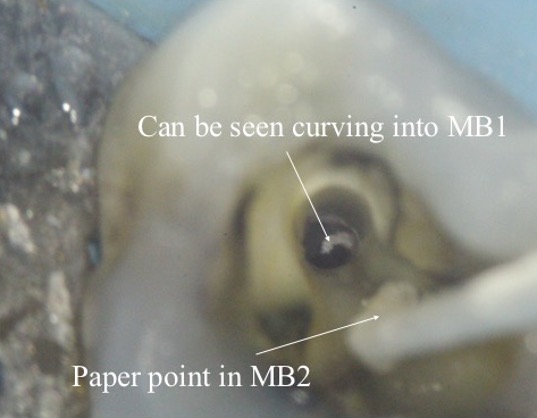
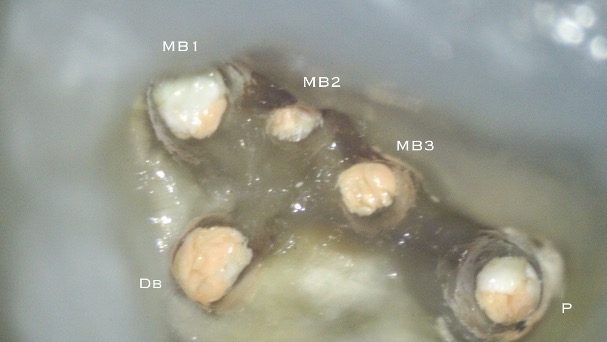
Figure 4: Patient was referred for the root canal retreatment of UR6. The tooth had been treated privately with her general dentist three years ago; the root canal treatment had been carried out to a good standard (under rubber dam isolation, three canals cleaned, shaped, disinfected using sodium hypochlorite and obturated to length). The patient did not have significant pain but the tooth did not ‘feel right’ and was affecting her function. Root canal retreatment was carried out and an additional MB2 canal was located. The patient’s symptoms settled immediately following treatment and she was advised to proceed with a cuspal coverage restoration.
Cone beam CT has become a very useful tool in endodontics. It allows us to see root canal morphology in three dimensions. It is important to note there are large differences in scan quality obtained by various CBCT machines; a high-resolution small volume scan is necessary to visualise the fine details required for endodontics.
CBCT has been shown to be a reliable tool for detecting MB2 canals and assessing their path up the root (Figure 5). However, studies show MB2 canals are still sometimes located clinically even when they are not seen on the scan (Blattner et al, 2010; Parker et al, 2017).
Location
Magnification and lighting make all the difference when trying to locate MB2. Studies have shown that the frequency of MB2 canal detection with microscope, dental loupes and no magnification were 71.1%, 62.5% and 17.2% respectively (Buhrley et al, 2002). The experience of the operator and time spent searching for the canal are also important factors.
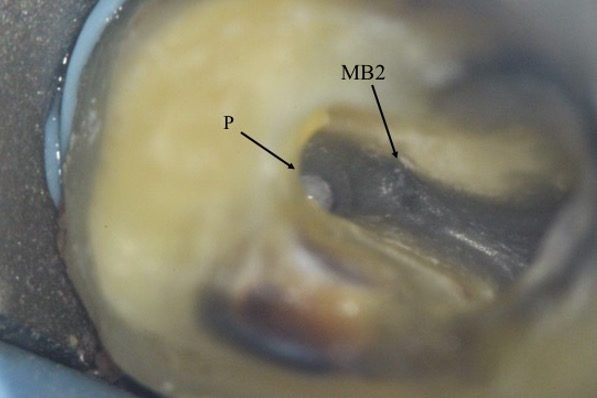
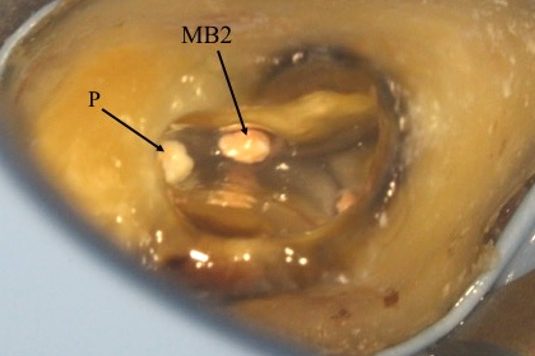
The pulp floor has developmental root fusion lines that are darker; these can provide a road map for locating canals, because the orifices lie at the terminus of these lines (Krasner and Rankow, 2004). The MB2 canal is commonly located within the developmental groove between MB1 and palatal orifices. Envisage a line joining the MB1 and palatal canal, and draw another line from DB to this line. In the majority of cases MB2 is located at this juncture, and a few millimetres away from the MB1 orifice (video and Figure 6).
A sharp DG16 probe is essential for exploring the area and locating the orifice. Less frequently, the MB2 orifice can lie closer to the palatal orifice (Figure 7) or within the MB1 orifice itself (Figure 8).
The orifice lies at the junction of the pulp floor and mesial wall, and is frequently covered by a mesial lip or ‘shelf’ of dentine, particularly in older patients. Therefore, the access cavity will need to be extended to remove this.
In calcified cases, the MB2 may be slightly deeper apically. Piezo-electric ultrasonic tips or long-neck burs used in a slow handpiece are very useful removing the dentine shelf and searching for MB2. They allow good vision during preparation because the head of the handpiece does not obstruct your view. They also remove dentine and calcifications in a controlled manner so the preparation is more conservative. It is essential to preserve as much dentine as possible because it is quite easy to perforate the mesial wall or pulp floor when searching for the MB2 (Figure 9).
Figure 6: locating the MB2 orifice
-
-
-
- i) Draw a line from MB1 to P. ii) Draw another line from DB to this line. The MB2 orifice normally lies at the juncture of these two lines
- MB2 located with a hand file
- Orifice enlargement and coronal flaring
- After cleaning and shaping.
-
-
Figure 7: MB2 is located in a more unusual position and closer to the palatal canal
- MB2 orifice detected close to the palatal canal
- After obturation.
Figure 8: MB2 is located in a more unusual position within the MB1 orifice
- Preoperative radiograph. The tooth had previously been accessed by the referral dentist
- MB2 was located within the MB1 orifice (mesial wall). The microscope photograph was taken after the MB1 and MB2 have been fully prepared
- Master cone radiographs taken with a GP cone in MB1
- Master cone radiograph taken with cone in MB2
- Mid-fill radiograph shows MB1 and MB2 are separate canals
- Postoperative radiograph
- Post-obturation photograph showing one MB orifice. A trough line can be seen where MB2 was searched for in its ‘typical’ location.
Figure 9: Patient referred for root canal retreatment of a maxillary first molar. There was a perforation noted where the dentist had searched for MB2. There was a GP point within the perforation
- Access regained: the GP point was removed to reveal the perforation on the pulp floor
- The true MB2 canal was located using a small hand file
- Canals prepared and obturated
- Perforation repaired using biodentine.
Instrumentation
I strongly advise fully preparing the MB1 canal prior to locating and instrumenting MB2. The MB2 often joins MB1 at a sharp angle. It makes negotiation much easier if the MB1 is already enlarged (Figure 10).
Figure 10: Two cases showing MB2 joining MB1 in the mid-third of the root
- Master cone shows MB2 joining MB1
- MB2 joins MB1 at an acute curvature (white arrow).
Instrumentation of MB2 can often be difficult. The canal often has an abrupt mesial curvature in the coronal 1-3mm making it challenging to negotiate initially. I find that spending time initially gaining correct access and coronal flaring to gain straight line access can prevent ledges, which once formed are very difficult to bypass. Rotary orifice openers such as XA (by Dentsply Sirona) used in a brushing motion away from the furcation are very useful for this.
Small hand files (sizes 8-10) can then be taken further into the canal and a glide path formed prior to using rotary instruments. If at any point the hand file meets resistance the canal can be flared up to this point prior to taking pre-curved hand files back into the canal. The MB2 can be calcified in extensively restored teeth and older patients. Stiffer hand files and 17% EDTA solution can be very useful for these situations but care needs to be taken as it is also easy to ledge the canal using these.
The MB root is a small root and a more conservative preparation of the MB2 is necessary to prevent unnecessary weakening and fracture long term. I would recommend using a slightly less tapered (≦6%) rotary file for the final preparation. Some clinicians advise preparing MB2 to the level it joins MB1 to conserve dentine. However, in my experience I find the MB2 frequently joins MB1 but then separates into its own canal apically (2-1-2 morphology) (Figure 11). Therefore, I would recommend always preparing the MB2 to full length. Obturation of these complicated systems presents its own challenge and can only be done effectively using a warm technique.
Figure 11: Complex MB1/MB2 anatomy (2-1-2 morphology)
- Preoperative radiograph
- A paper point has been placed in MB2, and can be seen appearing in MB1 where the canals join
- Mid-fill radiograph showing the MB2 has a separate apical foramen from MB1. The MB1 and MB2 have a 2-1-2 morphology (two orifices-merging into one canal – separating into two canals). The MB2 should always be fully instrumented because this anatomy is difficult to predict
- Postoperative radiograph
- Microscope photograph.
Summary
Successful root canal treatment involves treating all the canals present. The MB2 has been shown to be present in most maxillary molars and the clinician should approach treatment of these teeth with this in mind. The MB2 is notoriously challenging to locate and negotiate, but with the correct magnification, light, equipment, knowledge and experience it can be treated predictably.
References
Blattner TC, George N, Lee CC, Kumar V and Yelton CD (2010) Efficacy of cone beam computed tomography as a modality to accurately identify the presence of second mesiobuccal canals in maxillary first and second molars: a pilot study. J Endod 36(5): 867–70
Buhrley LJ, Barrows MJ, BeGole EA and Wenckus CS (2002) Effect of magnification on locating the MB2 canal in maxillary molars. J Endod 28(4): 324-7
Krasner P and Rankow HJ (2004) Anatomy of the pulp-chamber floor. J Endod 30(1): 5-16
Parker J, Mol A, Rivera EM and Tawil P (2017) CBCT uses in clinical endodontics: the effect of CBCT on the ability to locate MB2 canals in maxillary molars. Int Endod J 50(12): 1109-15