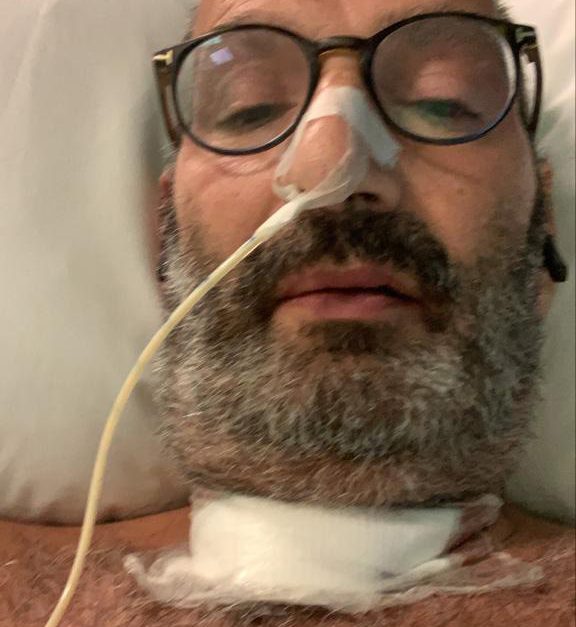
 Tony Jacobs reflects on his harrowing near-death experience after admitting to ICU with COVID-19 and his recovery from the virus since.
Tony Jacobs reflects on his harrowing near-death experience after admitting to ICU with COVID-19 and his recovery from the virus since.
Very simply, I feel it was touch and go that I am able to be here to write this article about my experience with COVID.
It was far worse for my close family, and all the people around me. They knew what was happening. I was unaware and retain the amnesia that comes with the ICU medications.
Where did we catch COVID?
My illness started with the classic symptom of a continuous cough. This commenced in the middle of a working day in mid-March, just after muted celebrations of a happy occasion, my 40th wedding anniversary with Lesley, who is now a retired headteacher.
I think that is quite a milestone, quite an achievement. We had plans for more celebrations with family in April and May. Those have all remained suspended for now.
I do feel I caught the virus from a patient in the week prior, but I cannot identify whom, and I have not tried.
If the person emerges I wonder how I will feel? It won’t be anger, but perhaps curiosity will one day lead me to find out from the day lists of that period.
We all used to shake hands – perhaps that was the transmission method.
How it began
Our first few days of the virus were at home in Manchester. My wife started with the effects on the same day.
Some days she was worse than me, and after about a week, she was improving. I went downhill.
I sought medical advice one evening and treatment at that time was paracetamol. By the next day, I was much worse.
I woke and showered, then returned to sit on the bed and apparently I could not find the strength to dress myself. This was when Lesley realised more help was needed.
Phone calls led us to a process of attending our local general hospital. Here my wife had to leave me in their A&E, and a quick test showed my oxygen saturation to be 80% – no wonder I had no energy!
Quite soon I was on a ventilator, and from there into ICU, and an induced coma. I can vaguely recall Lesley coming in for a conversation with the respiratory consultant. Those were not the times for informed consent. They were doing their best to save a life, they certainly did not know then what they were dealing with. Their name for the condition is acute respiratory distress syndrome (ARDS).
Life in ICU
The nature of the drugs given causes amnesia for the patient. So the next four weeks left me with few memories.
I now know the team treated me with oxygen whilst proning. In this position, they gave me drugs to paralyse me.
At this stage some of the anaesthetic drugs ran out, across the whole of the UK. So again, the teams in ICU had to improvise with medications.
More information I’ve since learnt – I was the ninth to enter ICU in this general hospital. The first eight all developed kidney failure – another reason to be grateful for my recovery.
The maxillofacial team performed a tracheostomy, which was novel for COVID sufferers. They usually use it in long-term intubation. This wound has healed well – it needed special nursing initially.
Returning home after COVID
When we see people leaving the hospitals after COVID, we see them in a wheelchair. The simple reason is the effects of the ICU leaves one unable to walk.
A person loses about 3% of muscle mass for each day in the ICU. So my loss was around 60%, and it took me some time to learn to walk again, and to gain the strength to get out of bed!
I had a few days of recuperation with help from physiotherapists in getting me walking and testing I could climb and descend a flight of stairs.
Discharge from the hospital created an emotional day. Hugging and holding Lesley, then children and grandchildren waiting in the street along with many neighbours. This time was still the height of lockdown, late April, when many forged new community spirit. For example, a small army of volunteers would offer to shop daily for us.
Like many others, our neighbours have now created a stronger bond, with regular evening meetings at a suitable social distance.
Milestones along the way of recuperation have been walking unaided, but with difficulty in balancing to start. And 15 weeks later, I can walk further but balance remains impaired.

After effects
I am lucky, compared to others, that I have few side effects in recuperation. There are long lists of post-COVID symptoms. I have seen the phrase ‘long-tail COVID’.
My main problem has been peripheral neuropathy of my lower limbs, numbness and severe pain from the knee downwards. I have had various medications for this, and these have had varied success, and varied side effects.
From mid June to end of July, my GP and I spent weeks trying to adjust my medications to find the true cause of the medication side effects. I think we have the balance right now. And the winning pain relief seems to be pregabalin.
Other aspects of recuperation are regaining a normal sleep pattern, this took a good 10 weeks.
In addition, the ICU experience led to multiple dreams, fantasies and hallucinations, and they seemed very real to me, both at the time, and afterwards. Even now, I can recall the dreams and their reality. But I have been gradually able to separate what is real and what was fantasy.
Heartfelt thanks
I hope that when I look back in a year or two and beyond, I will realise this episode is a short part of my life and I can forget it.
I have been able to keep in touch with some other local survivors, and we have had many phone conversations. This includes a dental colleague from north Yorkshire.
I do believe mutual support from people with a similar tale to tell is helpful.
If any other dental colleagues reading this wish to speak, I am happy to spend time and hear your story. Please contact me via my dental website GDPUK.
One last thought – my story here. This should lead you to: www.gofundme.com/f/thank-you-to-the-team-who-looked-after-tony-jacobs.
I must close with my heartfelt thanks! Thanks to the teams and teams of hospital workers who helped to save my life from this unknown virus that has swept the world.


