Guvinder Gakhal explains how he managed a case of severe tooth wear using SprintRay 3D-printed crown resin and techniques learned on Avant Garde’s education programme.
This clinical case has been developed and executed with the support of Avant Garde workflows and laboratory services, ensuring precision and excellence at every stage. Having attended Avant Garde’s education program, Dr Guvinder Gakhal has applied these principles and techniques throughout the treatment process. With great pride, he is pleased to share the following case, demonstrating how structured workflows and advanced lab collaboration can elevate both clinical outcomes and patient satisfaction.
This case report describes the full-mouth rehabilitation of a patient presenting with generalised tooth wear, restored using SprintRay’s 3D-printed crown resin technology. The treatment followed a structured digital workflow, including diagnostic planning, a trial smile, crown lengthening, and fabrication of definitive restorations via 3D printing. The minimally invasive approach provided predictable functional and aesthetic outcomes with improved patient comfort and efficiency. This case highlights the potential of 3D-printed definitive restorations as a viable alternative to conventional methods in complex rehabilitation cases.
Initial presentation
A male 56-year-old presented with generalised tooth wear and has been a long-standing patient of the practice. He reported no pain or concerns until the extensive wear was highlighted in his examination.
He revealed that he has suffered nocturnal bruxism for many years and has noticed that his teeth have noticeably gotten shorter over the years believing that it was due to natural ‘wear and tear’.
Taking a patient-centred approach, we discussed and highlighted his teeth were at high risk of complete loss of clinical height and pulp involvement. If left unprotected and subsequently required extraction, there would be little room for implants or dentures owing to the alveolar compensation. Thus restoring the dentition in the patient’s later years would prove extremely challenging.


Patient history
- Age: 56
- Gender: male
- Occupation: electrician
- Parafunction: evident in generalised tooth wear from nocturnal bruxism and hypertrophic masseters
- No reports of TMJD or abnormalities
- General health: no medical issues.
Other challenges
- Alveolar compensation, maintaining occlusal vertical dimension (OVD)
- Shortened clinical crowns with pulp exposure imminent on lower anteriors
- Asymmetrical gingival zeniths
- Buccally positioned canines.
After discussing the above issues with the patient and understanding their own desire, expectations and limitations it was decided to:
- Protect remaining tooth structure by adding restorative material
- Increase the OVD to allow for adequate material thickness and keep the treatment minimally invasive
- Avoid any unnecessary reductions to tooth tissue
- Improve crown height on uppers and zeniths to allow for better aesthetics.
- Declined lower osseous crown-lengthening due to concerns of healing and adaptation
- Keep aesthetics as natural as possible to avoid the look of ‘having work done’.


Treatment plan
- Surgical Crown lengthening of upper 2-2
- Allow healing for 3/12
- Trial smile
- Final fit
- Occlusal guard to protect upper anteriors.
Trial smile
- Digital design of wax-up was designed using the Avant Garde portal and transferred using bisacryl resin (Luxatemp shade A3)
- The mock up was used to assess occlusion, OVD and speech. This was accepted by the patient.
- Final design was accepted and communicated to the lab which involved little to no modification.
Why opt for 3D printed?
Traditionally, composite resin would be a preferred method to restore the dentition owing to its repairability, preservation of tooth tissue and wear rate. We were cautious of the use of ceramic restorations in this case due to fracture risks, unpredictable repair and budget.
At the time of writing, our clinical success using Srintray Bego A3 crown resin on single units had been so far predictable, successful and extremely accurate. The technology is relatively new and hence the need for long-term testing is required. The patient was keen to partake in assessing its performance, longevity and viability as a solution to wear cases for future patients.
In this case, 3D printed restorations were selected over composite due to: Accuracy of fit, ceramic reinforcement and cad designs that precisely match the mock-up trial. This would in theory provide accurate marginal adaptation, functional accuracy, repairability and superior strength over composite.
Printing of the 3D restorations and lab work
- STL files sent to Sprintray Pro 2 printer
- Hand cleaned with 99% IPA
- Candy coated
- Final cure with nanocure
- Polished and tried in.
Cementation protocol
Try-in
- Try-in in using glycerine and assessed for marginal fit and contacts, afterwards the restorations were air abraded using cojet sand
- Cleaned using Ivoclean universal cleaner
- Primed using Scotchbond universal plus (SBU+) and Rely x Universal translucent (RXUT).
Tooth preparation
- Sandblasted with cojet, etched with prophoric acid 37% for 15s, air dried and primed using SBU+.
Cementation of final restorations
- Cemented using RXUT, tac cured and excess cleaned with floss, tepes and hand scaler tip
- Final cure under glycerine
- Occlusion checked using shimstock foil 8 micron and articulating paper 20 micron to ensure both safe static and dynamic occlusal movements.
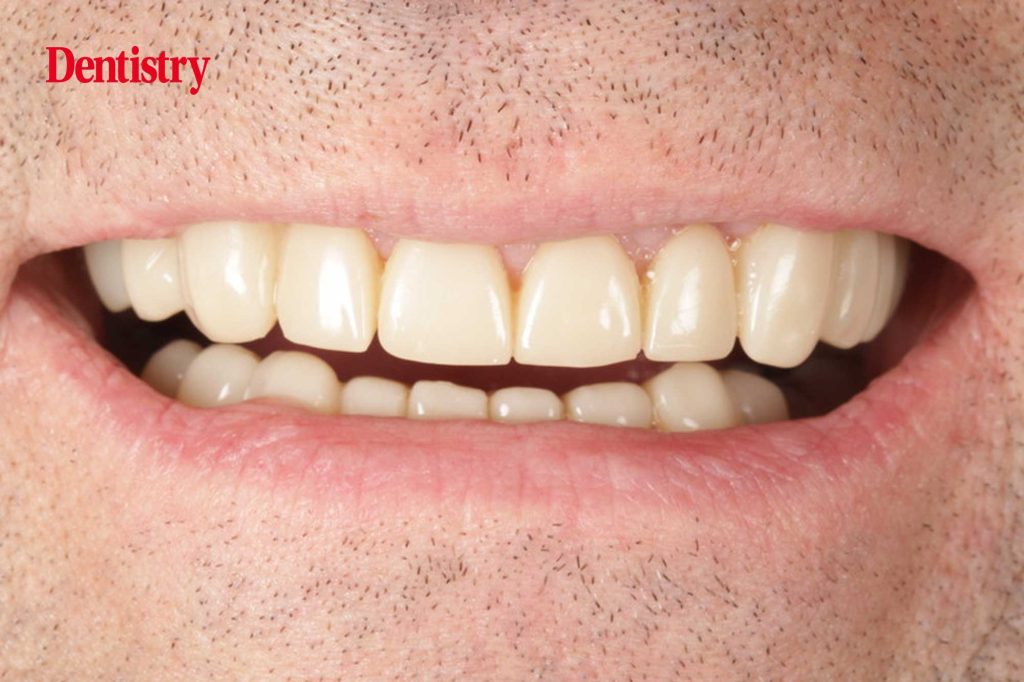
Final outcome
- Patient was extremely happy with the immediate final aesthetic result and reported no issues with adapting to the new OVD and restorations over the subsequent weeks.
- He was reviewed at two weeks, one month, two months and finally three months, and was delighted with no concerns.


Reflection and learning outcomes
Both the team at Avant Garde Laboratories and I are delighted with the result and provide confidence in treating complex cases with 3D Printed materials. The digital design workflow allowed us to be efficient and precise as we were able to share ideas, print models and restorations without delay.
Minimally invasive preparations and biological preservation meant no tooth was prepped into dentine that was already exposed. We managed to preserve significant amounts of enamel for bonding and reducing risk of pulpal flare up.
The case was successful owing to our Patient-centered approach and open communication throughout.


We have incorporated the Sprintray workflow into wear cases for those who seek an affordable solution and aid us in reviewing its performance. Since this case, ceramic dominant resins have been approved for use which will offer stronger restorations and still offer the advantages of repair, accuracy and modification.
There is limited studies and evidence available at present. More structured research is required in the performance of these new materials and long-term follow ups. This anecdotal approach to wear cases is to be used with caution. The rationale for this treatment was based on thorough patient assessment, understanding the properties of the materials, their workflows and patient selection.
Acknowledgements
This case would not have been possible without the support of the following people:
- Avant Garde Dentistry for its education on solution based workflows
- John and the team at Avant Garde Labs
- My team at Riverside Dental Practice (Stafford) who have embraced and developed alongside our new technology. In particular, Grace Francis for processing print outs and polishing the final restorations which proved to be a steep learning curve for us all!
- Attiq Rehman at Precision Academy for his clear and simplistic teaching of the principles of occlusion, preparation designs, cementation protocols and pitfalls to watch out for.
This article is sponsored by Dental Excellence.

