 Kris Leeson and Rob Lewis describe the patient workflow through their practice and explain how to keep patients and the dental team safe.
Kris Leeson and Rob Lewis describe the patient workflow through their practice and explain how to keep patients and the dental team safe.
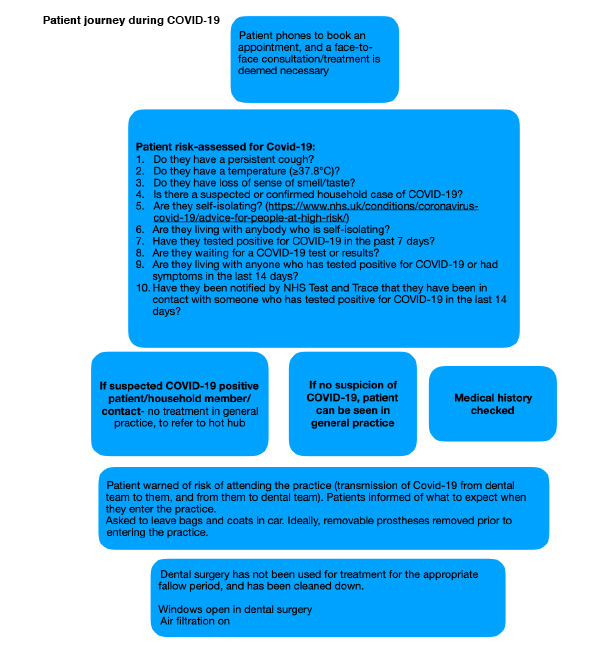
The introduction of a new standard operating procedure (SOP) on 4 June 2020 outlines how dental practices can begin to see patients again. One of the areas discussed in this document is the way we have created a patient journey. This is a protocol for planning patients’ movements through the practice before, during and after their appointments. This aims to promote social distancing, minimise face-to-face interaction with others, and promote efficient entry and exit of the practice. Thereby maximising patient and staff safety.
Before the patient arrives
Practices should triage patients over the phone by the dental team. Perhaps send photographs of any issues they may have to the practice to help remote treatment planning.
This telephone call is an opportunity to update the patient’s medical history, carry out a COVID-19 risk assessment, and discuss likely treatment options. It is also an opportunity to build rapport with patients not well known to the clinician. And to explain the protocols put in place due to the pandemic.
The FGDP guidance suggests sending patients a ‘digital pre-appointment pack’. This can include things like consent forms for patients to fill out remotely. Time spent in this pre-appointment phase will mean that face-to-face contact can be kept to a minimum during the appointment.
Practices should also clear any unnecessary ‘clutter’, such as magazines and plants.
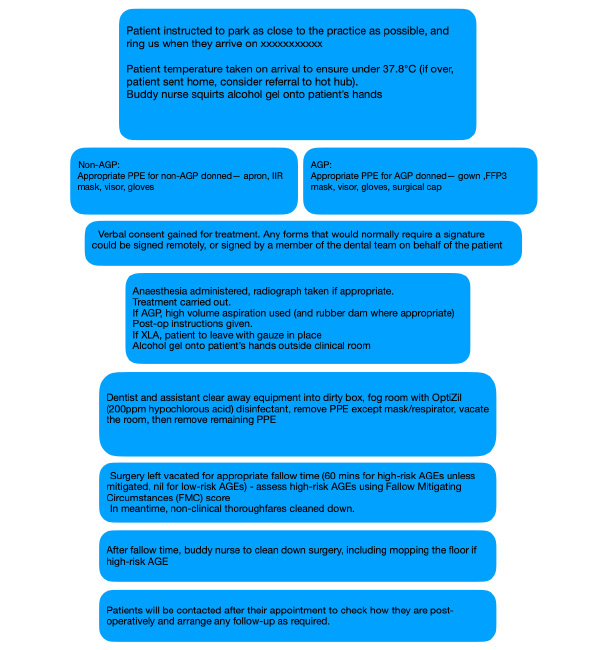
Upon arrival
The reception team should contact the patient on the day of their appointment to repeat the COVID-19 risk assessment. The practice entrance should remain locked.
Patients should contact the practice by telephone when they arrive. The practice may ask them to wait in their car or stand outside the practice, maintaining social distancing. Where this is not practical, dental practices should consider zoning their waiting room. So that patients remain 2m apart from others.
Carefully plan the appointment diary to minimise the total number of patients present in the practice at any given time.
You should see shielded patients who require a face-to-face appointment early in the morning to maximise fallow time from the previous day. Encourage patients not to bring bags or coats into the practice, and to use the bathroom at home before their arrival. They should arrive promptly for their appointment, and not too early.
Patients should only enter the practice when invited to by a member of the dental team. Practices can make it clear that all attendances are by appointment only.
A ‘buddy nurse’ can greet the patient wearing the following PPE:
- Fluid-resistant surgical mask (FRSM)
- Visor
- Waterproof apron
- Gloves.
Practices may consider the use of a contactless thermometer to record the patient’s temperature, although this is not essential.
The buddy nurse asks the patient to apply hand sanitiser and explains how to do it. Encourage the patient not to touch anything in the practice if possible.
You can then escort the patient to the clinical room (or waiting area as appropriate). The buddy nurse will wipe down surfaces such as hand rails and door handles passed by the patient on their way in.
The appointment
After guiding the patient to the clinic room, the buddy nurse will open the door for the patient. The clinical team will greet the patient.
Again, the buddy nurse will wipe down any surfaces which the patient may have inadvertently touched.
The buddy nurse remains within earshot of the clinical room. Once the appointment is completed, the clinician can call the buddy nurse to open the door for the patient. Remind the patient not to touch anything on their way out.
Leaving the practice
The buddy nurse will again dispense hand sanitiser into the patient’s hands immediately after they leave the clinical area.
They will escort the patient out of the building, ensuring that the exit route is clear of other patients, or staff members not wearing PPE who are less than 2m from the patient.
Practices should consider a one-way flow of patients, so that patients enter and exit the building via different doorways.
Surgery clean down and fallow time
After the patient leaves the surgery, the dentist and assistant will tidy away all instruments and put them into a sealed container. Fogging could be considered, using hypochlorus acid (200ppm) with the windows remaining open. Doff gloves (and gowns) in the surgery, although keep the face mask on at all times.
The surgery fallow time starts from the last aerosol generation within the surgery. The clinical team can record this.
All treatment rooms need to have a risk assessment to help decide the appropriate fallow time needed before the surgery can be mopped and all surfaces cleaned.
We have formulated the Fallow Mitigating Circumstances (FMC) score to help (Figure 1). We use this to determine fallow time using a weighted scoring system. Highest scores are allocated to mitigating circumstances that are most likely to reduce the fallow time. For example, the use of rubber dam has been shown to significantly reduce the number of microorganisms present in dental aerosol by 90-98% (Cochran, Miller and Sheldrake, 1989). Opening windows will increase air flow within the room, therefore further reducing fallow time significantly (Tang et al, 2006).
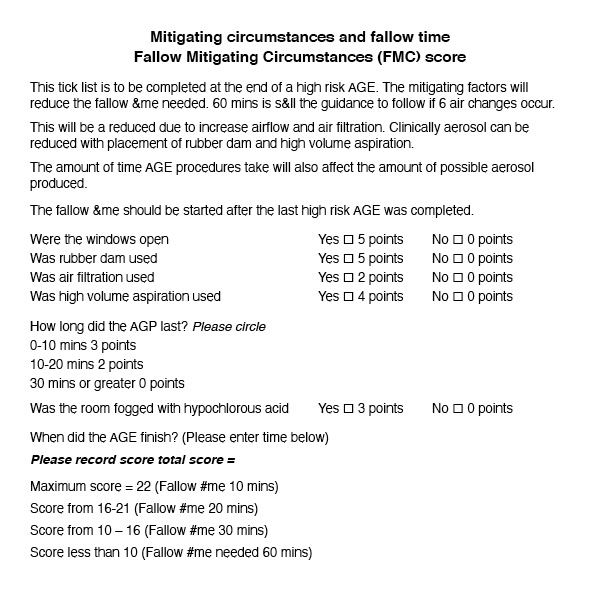
Unfortunately, there is currently very little evidence for fogging and air filtration systems so these have been scored lower. As evidence emerges this scoring system may be modified.
Maintaining social distancing
Zone communal areas with tape spaced in 2m intervals to promote social distancing, a method adopted by many supermarkets currently.
Staff members likely to come within 2m of patients should wear appropriate PPE. This means reception staff wearing an FRSM. The use of perspex screens on the reception desk also protects staff and patients from droplet spread (5).
Forms that the patient cannot sign remotely could be signed ‘COVID-19’ on the patient’s behalf. Consider remote payments over the telephone.
Other considerations
Signage of the rooms within the practice helps patients and staff to know where they can and cannot go. Arrows are helpful to further guide patients into and out of the practice safely.
Posters encourage and explain hand hygiene. The buddy nurse can show patients how to use hand sanitise properly. Hand sanitiser should be readily available at entry and exit points and outside the clinical areas.
Conclusion
Each practice will have to tailor its own patient journey. It will therefore likely require a few trial walk-throughs to iron out any creases.
Input from all members of the team is important, as is patient feedback. This way you can refine the journey to make it as effective as possible.
References
Cochran MA, Miller CH and Sheldrake MA (1989) The Efficacy of the Rubber Dam as a Barrier to the Spread of Microorganisms During Dental Treatment. J Am Dent Assoc 119(1): 141-4
Tang JW, Li Y, Eames I, Chan PKS and Ridgway GL (2006) Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. Journal of Hospital Infection 64(2): 100-14
View the other 10 steps back to practice after COVID-19
- Staff training
- Encouraging patients back
- Patient workflow
- PPE
- Communication
- Vulnerable patients
- Mental health
- Virtual consultations
- Looking forward
- Growing revenue.
 Kris Leeson is the practice principle of Thorpe Dental Group, based in York. He has an interest in dental implants and digital dentistry.
Kris Leeson is the practice principle of Thorpe Dental Group, based in York. He has an interest in dental implants and digital dentistry.
Rob Lewis is an associate dentist working at Woodthorpe Dental Centre on York. He is currently undertaking an MSc in periodontology.


